Organizational Needs Assessment NR703
Organizational Needs Assessment NR703
Organizational Needs Assessment NR703
NR703 Week 2 Organizational Needs Assessment
Assignment
Purpose
The purpose of this assignment is to identify a practice problem based on an organizational needs assessment, including the identification of the practice gap and formulation of the practice question. This assignment will allow for the assimilation of professional leadership competencies in project management as a DNP-prepared nurse. Assignment content supports professional formation, communication, and dissemination skills relevant to the DNP-prepared nurse.
Please note that this is the first part of a 3-part assignment submitted in Weeks 2, 5, and 7. You will receive corrective feedback from your course faculty on the Week 2 and Week 5 assignments that you will use to prepare the Week 7 assignment.
Also Read:
NR703 Week 3 Leading Interprofessional Teams Discussion
NOTE: All NR703 assignments and their requirements should be discussed in relation to your proposed or hypothetical DNP practicum project. **No DNP practicum project will be approved for implementation until the second practicum course, NR-705 Project & Practicum II
Instructions
Complete the Organizational Needs Assessment: Practice Gap Identification Table on a healthcare organization of your choice. This will be submitted as Table 1.
- Link (Word doc): Organizational Needs Assessment: Practice Gap Identification TemplateLinks to an external site.
Include the following in your paper:
- Introduction
- Introduce the topic and establish the importance of an organizational needs assessment.
- Present a clear purpose statement.
- Create an organizing (outline) statement for the paper that matches the required level 1 headings (except for listing the conclusion).
- Problem: Using the information that you gathered on the Organizational Needs Assessment: Practice Gap Identification (Table 1), describe the practice problem by explaining these elements:
- Describe a specific location (hospital unit, community health clinic, surgical suite, primary care practice).
- Identify the key stakeholders (decision-makers).
- Explain the practice problem as would be identified by the stakeholders.
- Practice Gap
- In 1-2 organized paragraphs, summarize your findings in table 1, the Organizational Needs Assessment: Practice Gap Identification. Ensure the table is placed after the reference list starting on its own page with the heading Table 1.
- Practice Question: Define and briefly explain the project’s intended population, evidence-based intervention, and measurable outcomes (PICOT):
- Population: Describe the specific characteristics of the population that is the focus of the intervention.
- Intervention: Citing evidence listed in the Johns Hopkins Individual Evidence Summary Tool (Table 2) which was initiated in NR-716, describe the evidence-based intervention. There should be a total of three (3) references listed in Table 2 for this assignment. If necessary, add one research study or systematic review to support your intervention unless one already exists on the table from your previous courses.
- Comparison: State “compared to current practice” for the purposes of this assignment.
- Create and explain specific outcome measurements based on the current evidence you have collected in the Johns Hopkins Individual Evidence Summary Tool (attached as Table 2). If needed, add one research study or systematic review that supports your proposed outcome measurements.
- The source can be the same one that was used to support the intervention as long as it speaks to measurable outcomes. There should be a total of three (3) references listed in Table 2 for this assignment.
- Time: Time frame for the project implementation. (Practicum projects are typically 8 – 10 weeks long).
- State the Practice Question. Example: (P) For the critical care team in X hospital’s ICU, (I) does the implementation of the medical sepsis protocol (C) compared to the current practice (O) reduce the incidence of medical sepsis diagnoses in ICU patients as measured before and after the intervention (T) over a 10-week period?
- Conclusion
- Recap the paper’s purpose statement and organizing (outlining) statement of the three level 1 headings (not including the conclusion).
- Draw major conclusions from the body of your paper.
- Summarize the importance of effective communication for the DNP-prepared nurse in performing the practice gap and problem identification.
- References
- Create the reference page.
- Ensure each reference has a matching citation.
- Include a minimum of three (3) scholarly references (all three references on the Johns Hopkins Table should be included).
- Tables
- Add the completed Table 1 & Table 2 after the reference list. For directions on how to copy a table in Microsoft Word go to the following link:
- Link (webpage): Move or Copy a TableLinks to an external site.
- Table 2, the Johns Hopkins Individual Evidence Summary Tool, is attached (after Table 1) & completely filled out with at least three (3) quantitative research studies at a minimum. (NOTE: a minimum of three [3] references should be included on the reference list, including those in Table 2).
- Add the completed Table 1 & Table 2 after the reference list. For directions on how to copy a table in Microsoft Word go to the following link:
Table 1: Organizational Needs Assessment: Practice Gap Identification
| What is currently happening in the practicum site that causes the problem? | What should be happening in the practicum site based on current evidence*? | What do the stakeholders (decision-makers) identify as the gap between what is currently happening and what should be happening (this is your practice gap)? | Why is there a gap in practice?
What factors are contributing to the gap in practice? |
What evidence* do you have to demonstrate there is a practice gap (e.g., NDNQI, AHRQ Quality Indicators, National Hospital Quality Measures, HCAHPS, Joint Commission ORYX®, etc.)? |
| *Reference & citation required. | ||||
| [Add text] | [Add text] | [Add text] | [Add text] | [Add text] |
| [Add text] | [Add text] | [Add text] | [Add text] | [Add text] |
PICOT Problem Statement:
P (Population – example: For critical care team in X hospital ICU…)
I (Intervention – example: Does the implementation of the medical sepsis protocol…)
C (Comparison – example: Compared to current practice). NOTE: “C” is most commonly used for research projects, not DNP translation science projects. “C,” or Comparison intervention, is implied for DNP projects, although you will see instances where the C does not apply.
O (Outcome, measurable – example: Reduce the incidence of medical sepsis in patients as measured before and after…)
T (Time – Usually 8-10 weeks for a DNP practicum project)
Review the rubric below for the grading criteria.
APA Guidelines
Use the current Publication Manual of the American Psychological Association (APA Manual) and the Chamberlain Guidelines for Writing Professional Papers: Graduate Programs (located in the Canvas Resources menu under the Writing Center) to complete this assignment. Follow these guidelines when completing each component. Contact your course faculty if you have questions.
- Use the standard APA Paper Template (located in the Canvas Resources: Writing Center) to format this assignment.
- Turn on Grammarly to check the correctness of the grammar and punctuation as you write. (Note: if you have not already done so, please download the free version at Grammarly.com before constructing the assignment.)
- Use the title, “Organizational Needs Assessment,” for your project and construct a title page using the APA paper template.
- Use the following prescribed Level 1 headings for this paper (do not include the outline letters):
- Problem
- Practice Gap
- Practice Question
- Conclusion
Writing Requirements (APA format)
- Length: 3-4 pages (not including title page, references page, or attachments)
- 1-inch margins
- Double-spaced pages
- 12-point Times New Roman
- Headings & subheadings
- In-text citations
- Title page
- Reference page
- Standard English usage and mechanics
- CARE Plan paragraph development structure
Program Competencies
This assignment enables the student to meet the following program competences:
- Applies organizational and system leadership skills to affect systemic changes in corporate culture and to promote continuous improvement in clinical outcomes. (PO 6)
- Appraises current information systems and technologies to improve health care. (POs 6, 7)
- Creates a supportive organizational culture for flourishing collaborative teams to facilitate clinical disease prevention and promote population health at all system levels. (PO 8)
Course Outcomes
This assignment enables the student to meet the following course outcomes:
- Compare and contrast theories of organizational behavior and leadership. (PCs 2, 4; PO6)
- Investigate the role of advanced nursing practice in innovation and transformation to propose solutions impacting healthcare systems. (PCs 2, 4; PO 6)
- Differentiate attributes of effective leaders and followers in influencing healthcare. (PCs 2, 4; PO 6)
- Formulate selected strategies for leadership and influence across healthcare systems. (PC 6; PO 8)
Due Date
- By 11:59 p.m. MT on Sunday
- Late Assignment Policy applies
Rubric
Organizational Needs Assessment NR703 Week 2 Assignment Grading Rubric
| W2 Assignment Grading Rubric | ||||||
| Criteria | Ratings | Pts | ||||
| This criterion is linked to a Learning Outcome Introduction
Requirements: |
|
10 pts | ||||
| This criterion is linked to a Learning Outcome Problem: Using the information that you gathered on the Organizational Needs Assessment: Practice Gap Identification (Table 1), describe the practice problem.
Requirements: |
|
30 pts | ||||
| This criterion is linked to a Learning Outcome Practice Gap
Requirements: 2. Include a thoroughly completed Organizational Needs Assessment: Practice Gap Identification Table as Table 1, placed after the reference list. |
|
30 pts | ||||
| This criterion is linked to a Learning Outcome Practice Question: Define and briefly explain the project’s intended population, evidence-based intervention, and measurable outcomes (PICO).
Requirements: |
|
40 pts | ||||
| This criterion is linked to a Learning Outcome Conclusion
Requirements: |
|
10 pts | ||||
| This criterion is linked to a Learning Outcome References
Requirements: |
|
10 pts | ||||
| This criterion is linked to a Learning Outcome APA Style and Organization for Scholarly Papers
Requirements: |
|
10 pts | ||||
| This criterion is linked to a Learning Outcome Clarity of Writing
Requirements: |
|
10 pts | ||||
| Total Points: 150 | ||||||
NR703 Week 2 Lesson 2 Leading through Translational Science Change Frameworks
Organizational Needs Assessment
A primary role of DNP-prepared nurses is translating evidence into practice. You have already been conceptualizing the topic areas you are interested in developing for your DNP practice change project and have begun collecting evidence for them in a Johns Hopkins Individual Evidence Summary Tool (Dang & Dearholt, 2018).
However, you may not have considered what your practicum site needs, which may not be what you have envisioned. That raises several questions.
- What do the stakeholders or practicum site decision-makers want you to do?
- What answers to practice gaps do stakeholders invested in your project need answered?
- Is the idea you have practical for the practicum site?
- Does the organization have a larger project or agenda that a DNP project might serve?
So, the first thing a DNP-prepared nurse must do to implement a practice change project is to understand what needs to be done and why. An organizational needs assessment is the foundational planning step that you must take for your DNP practice change project. Benjamin Franklin once said, “By failing to prepare, you are preparing to fail.” You cannot prepare unless you know what needs to be done, and that may not necessarily be what you have in mind.
As Yogi Berra once quipped, “If you don’t know where you’re going, you’ll end up someplace else.”
Many nurses conceptualize an organizational needs assessment by using the familiar nursing process format (ADPIE).
The needs assessment also drives the three primary conceptual project areas shown here in this Conceptual Project Portrait.
Conceptual Project Portrait Image Description
Practice Gap Identification
In this week’s assignment, you will construct an organizational needs assessment at a hypothetical practicum site. This will give you practice in performing the task and reinforce that a needs assessment to identify the practice gap is the foundational starting point for your practice change project. (Typical practicum sites include advanced practice setting, acute hospital care, LTC, community setting [church], health department, and home care.)
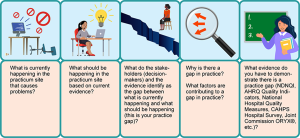
To perform a needs assessment with the practicum site stakeholders, use the following guide to help you understand what gaps are occurring between current practice and evidence-based practice.
Practice Gap Identification Image Description
Review the following examples:
| Practice Problem | What is currently happening in the practicum site that causes problems? | What should be happening in the practicum site based on current evidence? | What do the stakeholders (decision-makers) and the evidence identify as the gap between what is currently happening and what should be happening (this is your practice gap)? | Why is there a gap in practice? What factors are contributing to a gap in practice? | What evidence do you have to demonstrate there is a practice gap (NDNQI, AHRQ Quality Indicators, National Hospital Quality Measures, CAHPS Hospital Survey, Joint Commission ORYX®, etc.)? |
| Pediatric Practice | There are no clinical practice guidelines being used for the management of obese patients in a pediatric setting. | Nurse Practitioners (NPs) should be using evidence-based clinical practice guidelines to better manage children who are obese. | Approximately 40% of the patient population have been identified as being obese; however, there are no clear guidelines in place for the NPs to use/follow when planning patient care. | Potential issue with lack of knowledge associated with updated guidelines for pediatric obesity.
Physician-owned facility; potential lack of NP autonomy regarding practice. |
Comments provided by the NPs.
NPs report they want to be able to better manage and plan care for pediatric patients who are obese. National best-practice identifies that clinical practice guidelines should be used. Diagnostic indicators by incidence demonstrate an increase in obesity at this practice. |
| Long-Term Care Facility | The current practice for the prevention of unassisted falls is ineffective. | Unassisted falls, including falls with injuries, should not occur in the facility. | Stakeholders (particularly administrator, DON, & corporate governance) and ACHA survey results have established that there is an unacceptable rate of unassisted falls in the facility that is not being adequately addressed. | The current falls prevention process is not being followed.
Specifically, the gap in practice revealed · The initial fall risk factor assessment was not completed consistently. · Patients’ medications were not always reviewed for fall risk. · Patients with frequent toileting needs are not always assisted in a timely manner. |
MDS assessment data for falls
Nursing Home Compare (NHC) measures Internal QI data reports per unit Internal Falls Prevention Audit Risk Management data & litigation results |
NR703 Week 2 References
Bunting, M. (2016). The mindful leader: 7 practices for transforming your leadership, our organization and your life. John Wiley & Sons Australia, Ltd.
Dang, D., & Dearholt, S. (2018). Johns Hopkins nursing evidence-based practice: Model and guidelines. Sigma Theta Tau International.
Nadler, R., Carswell, J. J., & Minda, J. P. (2020). Online mindfulness training increases well-being, trait emotional intelligence, and workplace competency ratings: A randomized waitlist-controlled trial. Frontiers in Psychology, 11, 1-19. https://doi.org/10.3389/fpsyg.2020.00255
