NR703 Week 2 Assignment | Organizational Needs Assessment
NR703 Week 2 Assignment | Organizational Needs Assessment – Step-by-Step Guide With Example Solution
The first step before starting to write the NR703 Week 2 Assignment | Organizational Needs Assessment is to understand the requirements of the assignment. The first step is to read the assignment prompt carefully to identify the topic, the length and format requirements. You should go through the rubric provided so that you can understand what is needed to score the maximum points for each part of the assignment.
It is also important to identify the paper’s audience and purpose, as this will help you determine the tone and style to use throughout. You can then create a timeline to help you complete each stage of the paper, such as conducting research, writing the paper, and revising it to avoid last-minute stress before the deadline. After identifying the formatting style to be applied to the paper, such as APA, review its use, including writing citations and referencing the resources used. You should also review the formatting requirements for the title page and headings in the paper, as outlined by Chamberlain University.
How to Research and Prepare for NR703 Week 2 Assignment | Organizational Needs Assessment
The next step in preparing for your paper is to conduct research and identify the best sources to use to support your arguments. Identify a list of keywords related to your topic using various combinations. The first step is to visit the Chamberlain University library and search through its database using the important keywords related to your topic. You can also find books, peer-reviewed articles, and credible sources for your topic from the Chamberlain University Library, PubMed, JSTOR, ScienceDirect, SpringerLink, and Google Scholar. Ensure that you select the references that have been published in the last 5 years and go through each to check for credibility. Ensure that you obtain the references in the required format, such as APA, so that you can save time when creating the final reference list.
You can also group the references according to their themes that align with the outline of the paper. Go through each reference for its content and summarize the key concepts, arguments and findings for each source. You can write down your reflections on how each reference connects to the topic you are researching. After the above steps, you can develop a strong thesis that is clear, concise and arguable. Next, create a detailed outline of the paper to help you develop headings and subheadings for the content. Ensure that you plan what point will go into each paragraph.
How to Write the Introduction for NR703 Week 2 Assignment | Organizational Needs Assessment
The introduction of the paper is the most crucial part, as it helps provide the context of your work and determines whether the reader will be interested in reading through to the end. Begin with a hook, which will help capture the reader’s attention. You should contextualize the topic by offering the reader a concise overview of the topic you are writing about so that they may understand its importance. You should state what you aim to achieve with the paper. The last part of the introduction should be your thesis statement, which provides the main argument of the paper.
How to Write the Body for NR703 Week 2 Assignment | Organizational Needs Assessment
The body of the paper helps you to present your arguments and evidence to support your claims. You can use headings and subheadings developed in the paper’s outline to guide you on how to organize the body. Start each paragraph with a topic sentence to help the reader know what point you will be discussing in that paragraph. Support your claims using the evidence collected from the research, and ensure that you cite each source properly using in-text citations. You should analyze the evidence presented and explain its significance, as well as how it relates to the thesis statement. You should maintain a logical flow between paragraphs by using transition words and a flow of ideas.
How to Write the In-text Citations for NR703 Week 2 Assignment | Organizational Needs Assessment
In-text citations help readers give credit to the authors of the references they have used in their work. All ideas that have been borrowed from references, any statistics and direct quotes must be referenced properly. The name and date of publication of the paper should be included when writing an in-text citation. For example, in APA, after stating the information, you can put an in-text citation after the end of the sentence, such as (Smith, 2021). If you are quoting directly from a source, include the page number in the citation, for example (Smith, 2021, p. 15). Remember to also include a corresponding reference list at the end of your paper that provides full details of each source cited in your text. An example paragraph highlighting the use of in-text citations is as below:
“The integration of technology in nursing practice has significantly transformed patient care and improved health outcomes. According to Morelli et al. (2024), the use of electronic health records (EHRs) has streamlined communication among healthcare providers, allowing for more coordinated and efficient care delivery. Furthermore, Alawiye (2024) highlights that telehealth services have expanded access to care, particularly for patients in rural areas, thereby reducing barriers to treatment.”
How to Write the Conclusion for NR703 Week 2 Assignment | Organizational Needs Assessment
When writing the conclusion of the paper, start by restating your thesis, which helps remind the reader what your paper is about. Summarize the key points of the paper by restating them. Discuss the implications of your findings and your arguments. Conclude with a call to action that leaves a lasting impression on the reader or offers recommendations.
How to Format the Reference List for NR703 Week 2 Assignment | Organizational Needs Assessment
The reference helps provide the reader with the complete details of the sources you cited in the paper. The reference list should start with the title “References” on a new page. It should be aligned center and bolded. The references should be organized in an ascending order alphabetically, and each should have a hanging indent. If a source has no author, it should be alphabetized by the title of the work, ignoring any initial articles such as “A,” “An,” or “The.” If you have multiple works by the same author, list them in chronological order, starting with the earliest publication.
Each reference entry should include specific elements depending on the type of source. For books, include the author’s last name, first initial, publication year in parentheses, the title of the book in italics, the edition (if applicable), and the publisher’s name. For journal articles, include the author’s last name, first initial, publication year in parentheses, the title of the article (not italicized), the title of the journal in italics, the volume number in italics, the issue number in parentheses (if applicable), and the page range of the article. For online sources, include the DOI (Digital Object Identifier) or the URL at the end of the reference. An example reference list is as follows:
References
Morelli, S., Daniele, C., D’Avenio, G., Grigioni, M., & Giansanti, D. (2024). Optimizing telehealth: Leveraging Key Performance Indicators for enhanced telehealth and digital healthcare outcomes (Telemechron Study). Healthcare, 12(13), 1319. https://doi.org/10.3390/healthcare12131319
Alawiye, T. (2024). The impact of digital technology on healthcare delivery and patient outcomes. E-Health Telecommunication Systems and Networks, 13, 13-22. 10.4236/etsn.2024.132002.
NR703 Week 2 Assignment | Organizational Needs Assessment Instructions
Purpose
The purpose of this assignment is to identify a practice problem based on an organizational needs assessment, including the identification of the practice gap and formulation of the practice question. This assignment will allow for the assimilation of professional leadership competencies in project management as a DNP-prepared nurse. Assignment content supports professional formation, communication, and dissemination skills relevant to the DNP-prepared nurse.
Please note that this is the first part of a 3-part assignment submitted in Weeks 2, 5, and 7. You will receive corrective feedback from your course faculty on the Week 2 and Week 5 assignments that you will use to prepare the Week 7 assignment. Have a look at NR703 Week 3 Leading Interprofessional Teams Discussion.
NOTE: All NR703 assignments and their requirements should be discussed in relation to your proposed or hypothetical DNP practicum project. **No DNP practicum project will be approved for implementation until the second practicum course, NR-705 Project & Practicum II
Instructions
Complete the Organizational Needs Assessment: Practice Gap Identification Table on a healthcare organization of your choice. This will be submitted as Table 1.
- Link (Word doc): Organizational Needs Assessment: Practice Gap Identification Template.
Include the following in your paper:
- Introduction
- Introduce the topic and establish the importance of an organizational needs assessment.
- Present a clear purpose statement.
- Create an organizing (outline) statement for the paper that matches the required level 1 headings (except for listing the conclusion).
- Problem: Using the information that you gathered on the Organizational Needs Assessment: Practice Gap Identification (Table 1), describe the practice problem by explaining these elements:
- Describe a specific location (hospital unit, community health clinic, surgical suite, primary care practice).
- Identify the key stakeholders (decision-makers).
- Explain the practice problem as would be identified by the stakeholders.
- Practice Gap
- In 1-2 organized paragraphs, summarize your findings in table 1, the Organizational Needs Assessment: Practice Gap Identification. Ensure the table is placed after the reference list starting on its own page with the heading Table 1.
- Practice Question: Define and briefly explain the project’s intended population, evidence-based intervention, and measurable outcomes (PICOT):
- Population: Describe the specific characteristics of the population that is the focus of the intervention.
- Intervention: Citing evidence listed in the Johns Hopkins Individual Evidence Summary Tool (Table 2) which was initiated in NR-716, describe the evidence-based intervention. There should be a total of three (3) references listed in Table 2 for this assignment. If necessary, add one research study or systematic review to support your intervention unless one already exists on the table from your previous courses.
- Comparison: State “compared to current practice” for the purposes of this assignment.
- Create and explain specific outcome measurements based on the current evidence you have collected in the Johns Hopkins Individual Evidence Summary Tool (attached as Table 2). If needed, add one research study or systematic review that supports your proposed outcome measurements.
- The source can be the same one that was used to support the intervention as long as it speaks to measurable outcomes. There should be a total of three (3) references listed in Table 2 for this assignment.
- Time: Time frame for the project implementation. (Practicum projects are typically 8 – 10 weeks long).
- State the Practice Question. Example: (P) For the critical care team in X hospital’s ICU, (I) does the implementation of the medical sepsis protocol (C) compared to the current practice (O) reduce the incidence of medical sepsis diagnoses in ICU patients as measured before and after the intervention (T) over a 10-week period?
- Conclusion
- Recap the paper’s purpose statement and organizing (outlining) statement of the three level 1 headings (not including the conclusion).
- Draw major conclusions from the body of your paper.
- Summarize the importance of effective communication for the DNP-prepared nurse in performing the practice gap and problem identification.
- References
- Create the reference page.
- Ensure each reference has a matching citation.
- Include a minimum of three (3) scholarly references (all three references on the Johns Hopkins Table should be included).
- Tables
- Add the completed Table 1 & Table 2 after the reference list. For directions on how to copy a table in Microsoft Word go to the following link:
- Link (webpage): Move or Copy a Table.
- Table 2, the Johns Hopkins Individual Evidence Summary Tool, is attached (after Table 1) & completely filled out with at least three (3) quantitative research studies at a minimum. (NOTE: a minimum of three [3] references should be included on the reference list, including those in Table 2).
- Add the completed Table 1 & Table 2 after the reference list. For directions on how to copy a table in Microsoft Word go to the following link:
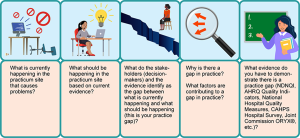
Table 1: Organizational Needs Assessment: Practice Gap Identification
| What is currently happening in the practicum site that causes the problem? | What should be happening in the practicum site based on current evidence*? | What do the stakeholders (decision-makers) identify as the gap between what is currently happening and what should be happening (this is your practice gap)? | Why is there a gap in practice?
What factors are contributing to the gap in practice? |
What evidence* do you have to demonstrate there is a practice gap (e.g., NDNQI, AHRQ Quality Indicators, National Hospital Quality Measures, HCAHPS, Joint Commission ORYX®, etc.)? |
| *Reference & citation required. | ||||
| [Add text] | [Add text] | [Add text] | [Add text] | [Add text] |
| [Add text] | [Add text] | [Add text] | [Add text] | [Add text] |
PICOT Problem Statement:
P (Population – example: For critical care team in X hospital ICU…)
I (Intervention – example: Does the implementation of the medical sepsis protocol…)
C (Comparison – example: Compared to current practice). NOTE: “C” is most commonly used for research projects, not DNP translation science projects. “C,” or Comparison intervention, is implied for DNP projects, although you will see instances where the C does not apply.
O (Outcome, measurable – example: Reduce the incidence of medical sepsis in patients as measured before and after…)
T (Time – Usually 8-10 weeks for a DNP practicum project)
Review the rubric below for the grading criteria.
APA Guidelines
Use the current Publication Manual of the American Psychological Association (APA Manual) and the Chamberlain Guidelines for Writing Professional Papers: Graduate Programs (located in the Canvas Resources menu under the Writing Center) to complete this assignment. Follow these guidelines when completing each component. Contact your course faculty if you have questions.
- Use the standard APA Paper Template (located in the Canvas Resources: Writing Center) to format this assignment.
- Turn on Grammarly to check the correctness of the grammar and punctuation as you write. (Note: if you have not already done so, please download the free version at Grammarly.com before constructing the assignment.)
- Use the title, “Organizational Needs Assessment,” for your project and construct a title page using the APA paper template.
- Use the following prescribed Level 1 headings for this paper (do not include the outline letters):
- Problem
- Practice Gap
- Practice Question
- Conclusion
Writing Requirements (APA format)
- Length: 3-4 pages (not including title page, references page, or attachments)
- 1-inch margins
- Double-spaced pages
- 12-point Times New Roman
- Headings & subheadings
- In-text citations
- Title page
- Reference page
- Standard English usage and mechanics
- CARE Plan paragraph development structure
Program Competencies
This assignment enables the student to meet the following program competencies:
- Applies organizational and system leadership skills to affect systemic changes in corporate culture and to promote continuous improvement in clinical outcomes. (PO 6)
- Appraises current information systems and technologies to improve health care. (POs 6, 7)
- Creates a supportive organizational culture for flourishing collaborative teams to facilitate clinical disease prevention and promote population health at all system levels. (PO 8)
Course Outcomes
This assignment enables the student to meet the following course outcomes:
- Compare and contrast theories of organizational behavior and leadership. (PCs 2, 4; PO6)
- Investigate the role of advanced nursing practice in innovation and transformation to propose solutions impacting healthcare systems. (PCs 2, 4; PO 6)
- Differentiate attributes of effective leaders and followers in influencing healthcare. (PCs 2, 4; PO 6)
- Formulate selected strategies for leadership and influence across healthcare systems. (PC 6; PO 8)
NR703 Week 2 Assignment | Organizational Needs Assessment Example
Organizational Needs Assessment
Organizations have diverse needs and challenges that hinder their ability to achieve their goals. An organizational needs assessment determines the barriers to achieving organizational goals and objectives, or identifies the needs gap between the current and desired outcomes. As DNP-prepared nurses, an organizational needs assessment is a must-have skill and competency for playing the project management role. The process of organizational needs assessment is an essential part of strategic planning, as the results of the needs assessment clarify current problems and inform the development of the appropriate solution. Additionally, an organizational needs assessment helps an organization focus on accomplishing strategic goals by identifying potential areas of improvement. The purpose of this essay is to present a practice problem based on an organizational needs assessment conducted on a long-term care facility, identify a practice gap, and develop a practice question. The paper’s outline includes the practice problem, the practice gap, and the practice question.
Organizational Practice Problem
The healthcare organization of focus is a long-term care facility. The long-term care facility is a medium-sized facility that serves a total of 500 patients. The facility offers patients comprehensive clinical care services, as well as social and physical support to facilitate their daily living. A large proportion of the patients in the long-term care facility are geriatric patients with terminal and chronic illnesses, ranging from diabetes, cancer, liver, and kidney diseases to psychiatric disorders. The institution has integrated long-term care and skilled nursing services to ensure it serves a broader range of patients, including those who do not require specialized clinical/medical services. The organization has skilled nurses, nurse aides, and other support staff to ensure it provides the best quality services to all patients.
The organizational needs assessment identified pressure ulcers as one of the significant practice problems affecting the organization. According to Cowan et al. (2019), pressure ulcers, also known as bed sores, are an injury to the skin and other underlying tissues due to prolonged pressure on the skin. Pressure ulcers are mainly caused by the immobility of a patient and the inability to change from a current position. Cowen et al. (2019) note that long-term care facilities have a high prevalence of pressure ulcers since most of their patients have neurodegenerative conditions and paraplegia, which increase immobility and the risk of pressure ulcers.
Various stakeholders are also the decision-makers in the long-term care facility. The decisions of these stakeholders significantly impact how the pressure ulcer practice problem is prevented, managed, controlled, and addressed. These stakeholders include nursing unit leaders, general managers, nurses, physicians, nurse aides, and institutional leaders. Research shows that nurses play a huge role in preventing, managing, and controlling pressure ulcers (Kim &Lee, 2019). Additionally, nurses collaborate with nursing unit leaders, managers, and institutional leadership to develop and suggest interventions to address pressure ulcers.
The procurement ulcers practice problem identified by stakeholders is a patient safety and care quality issue that significantly impacts patient outcomes and quality of life for patients. The problem is identified by the number of pressure ulcer cases reported within the organization and the associated costs of treating and managing these cases.
Practice Gap
A practice gap is an opportunity for improvement in practice or a deficit in existing skills, knowledge, and practice. Based on the assessment of organizational needs, the identified practice gap in the organization is the inadequacy of methods used to prevent pressure ulcers. A high number of pressure ulcer cases are reported within the organization, primarily due to inadequate prevention interventions. Ideally, long-term care facilities are expected to have low cases of pressure ulcers by ensuring high standards of intervention for pressure ulcer prevention are put in place. However, a practice gap is seen when there is a deficit in these interventions, and the facility reports a high number of pressure ulcer cases. The factors contributing to the practice gap include potential issues related to a lack of knowledge in pressure ulcer prevention and inadequate prevention measures within the organization. Evidence demonstrating the practice gap includes comments from nurses in the facility, pressure ulcer case reports, and nurse practitioners’ reports of a desire to play their part and prevent pressure ulcers more effectively.
Practice Question
The population of focus includes male and female patients admitted to the long-term care facility for more than six months. The recommended intervention is the use of ripple mattresses for preventing pressure ulcers. According to Shi et al. (2020), hospital bed and mattress interventions effectively prevent pressure ulcers in immobile patients. Research shows that ripple mattresses are one of the interventions that have been tested effectively in the treatment and prevention of pressure ulcers (Shi et al., 2021). The current practice to be considered for comparison is routine care with 2-hour repositioning. The outcome of the intervention is a reduction in the facility’s pressure ulcer cases. The project intervention will be implemented over a period of 10 weeks.
The practice question developed to address the practice gap is as follows: For patients hospitalized for more than six months, does the use of ripple mattresses, compared to routine care, reduce the number of new pressure ulcer cases as measured before and after the intervention in 10 weeks?
Conclusion
The organizational needs assessment of the long-term care facility identified pressure ulcers as a significant practice problem within the institution. The institution’s high number of pressure ulcer cases evidences the practice gap. The recommended intervention is the use of ripple mattresses. Effective communication is essential for the DNP-prepared nurse in identifying problems and recognizing practice gaps, as collaboration with the entire interprofessional team is necessary.
References
Cowan, L. J., Ahn, H., Flores, M., Yarrow, J., Barks, L. S., Garvan, C., Weaver, M. T., & Stechmiller, J. (2019). Pressure Ulcer Prevalence by Level of Paralysis in Patients With Spinal Cord Injury in Long-term Care. Advances in Skin & Wound Care, 32(3), 122–130. https://doi.org/10.1097/01.ASW.0000553109.70752.bf
Kim, J. Y., & Lee, Y. J. (2019). A study on the nursing knowledge, attitude, and performance towards pressure ulcer prevention among nurses in long‐term care facilities in Korea. International Wound Journal, 16, 29–35. https://doi.org/10.1111/iwj.13021
Shi, C., Dumville, J. C., Cullum, N., Rhodes, S., & McInnes, E. (2020). Beds and mattresses for treating pressure ulcers. The Cochrane Database of Systematic Reviews, 2020(5), CD013624. https://doi.org/10.1002/14651858.CD013624
Shi, C., Dumville, J. C., Cullum, N., Rhodes, S., McInnes, E., Goh, E. L., & Norman, G. (2021). Beds, overlays and mattresses for preventing and treating pressure ulcers: an overview of Cochrane Reviews and network meta‐analysis. The Cochrane Database of Systematic Reviews, 2021(8). https://doi.org/10.1002%2F14651858.CD013761.pub2
Table 1: Organizational Needs Assessment
|
What is currently happening in the practicum site? |
What should be happening at the practicum site? |
What is the gap between what is currently happening and what should be happening (this is your practice gap)?
|
Why is there a gap in practice? What factors are contributing to the gap in practice? |
What evidence do you have to demonstrate there is a practice gap? |
|
There is a high number of new pressure ulcer cases reported in the long-term care facility. |
Nurse Practitioners (NPs) should be using evidence-based pressure ulcer prevention strategies to reduce the number of new cases. |
Approximately 35% of the patient population has reported pressure ulcers; however, there are no clear pressure ulcer prevention guidelines, apart from routine care.
|
Potential issue with the lack of knowledge associated with pressure ulcer prevention
Inadequate prevention measures in the facility |
Comments provided by the Nurses.
NPs report that they want to be better able to prevent pressure ulcers, especially among elderly patients.
|
Table 2: Johns Hopkins individual evidence summary tool
Practice Question: For the patients hospitalized for more than six months, does the use of ripple mattresses, compared to routine care, reduce the number of new pressure ulcer cases as measured before and after the intervention in 10 weeks?
Date: 16th March
|
Article Number |
Author and Date |
Evidence Type |
Sample, Sample Size, Setting |
Findings That Help Answer the EBP Question |
Observable Measures |
Limitations |
Evidence Level, Quality |
|
2021 (8) |
Shi, C., Dumville, J. C., Cullum, N., Rhodes, S., McInnes, E., Goh, E. L., & Norman, G. (2021). |
Review of Meta-analyses |
4 reviews with 68 studies and 18174 participants |
Bed overlays and mattresses were found to be effective in preventing pressure ulcers as compared to routine care |
The article reviewed articles with bed overlays and mattresses, pressure ulcer prevention interventions |
Other prevention interventions were not considered in the comparisons |
Shi et al. (2021) was appraised as Level I evidence with a grade A quality. The study has generalizable results, and the sample size is sufficient for the study design. |
|
32(3) |
Cowan, L. J., Ahn, H., Flores, M., Yarrow, J., Barks, L. S., Garvan, C., Weaver, M. T., & Stechmiller, J. (2019). |
Quasi-experimental study |
7,540 patients with quadriplegia, 11,614 patients with paraplegia, and 32,510 patients with hemiplegia in LTC facilities. |
Patients with paraplegic issues are at a high risk of pressure ulcers, thus a need to implement prevention interventions |
The study aimed to assess the prevalence of pressure ulcers in long-term care facilities |
The study only focused on patients with paraplegic issues, leaving out other important factors such as neurodegenerative factors |
Cowan et al. (2019) were appraised at Level II grade A Quality. The sample size is sufficient, and the results are generalizable. |
|
2020 (5) |
Shi, C., Dumville, J. C., Cullum, N., Rhodes, S., & McInnes, E. (2020) |
Systematic review |
32 studies with 9038 participants from acute care settings |
Alternating pressure in ripple mattresses reduced the proportion of participants developing new pressure ulcers |
The observable measures included the prevalence of pressure ulcers and the number of new cases |
The studies included in the review have an average of 80 participants, which is a small number. The methods used in these studies were also likely to produce errors |
Shi et al. (2020) were appraised at level I grade B quality since the sample was inadequate |
|
16 |
Kim, J. Y., & Lee, Y. J. (2019) |
Experimental study |
282 registered nurses in long-term care facilities |
Nurses were found to play a significant role in the prevention of pressure ulcers using various nursing interventions |
Registered demonstrated a positive attitude, knowledge and skills toward the prevention of pressure ulcers |
The study’s primary limitation is the failure to include other factors of pressure ulcer prevention |
Kim and Lee (2019) were appraised at level II grade A quality The sample is adequate, and the results are generalizable to similar populations. |
