NURS-FPX6011 Assessment 1 Evidence-Based Patient-Centered Concept Map
NURS-FPX6011 Assessment 1 Evidence-Based Patient-Centered Concept Map – Step-by-Step Guide
The first step before starting to write the NURS-FPX6011 Assessment 1 Evidence-Based Patient-Centered Concept Map, it is essential to understand the requirements of the assignment. The first step is to read the assignment prompt carefully to identify the topic, the length and format requirements. You should go through the rubric provided so that you can understand what is needed to score the maximum points for each part of the assignment.
It is also important to identify the audience of the paper and its purpose so that it can help you determine the tone and style to use throughout. You can then create a timeline to help you complete each stage of the paper, such as conducting research, writing the paper, and revising it to avoid last-minute stress before the deadline. After identifying the formatting style to be applied to the paper, such as APA, you should review its use, such as writing citations and referencing the resources used. You should also review how to format the title page and the headings in the paper.
How to Research and Prepare for NURS-FPX6011 Assessment 1 Evidence-Based Patient-Centered Concept Map
The next step in preparing for your paper is to conduct research and identify the best sources to use to support your arguments. Identify the list of keywords from your topic using different combinations. The first step is to visit the university library and search through its database using the important keywords related to your topic. You can also find books, peer-reviewed articles, and credible sources for your topic from PubMed, JSTOR, ScienceDirect, SpringerLink, and Google Scholar. Ensure that you select the references that have been published in the last words and go through each to check for credibility. Ensure that you obtain the references in the required format, for example, in APA, so that you can save time when creating the final reference list.
You can also group the references according to their themes that align with the outline of the paper. Go through each reference for its content and summarize the key concepts, arguments and findings for each source. You can write down your reflections on how each reference connects to the topic you are researching about. After the above steps, you can develop a strong thesis that is clear, concise and arguable. Next you should create a detailed outline of the paper so that it can help you to create headings and subheadings to be used in the paper. Ensure that you plan what point will go into each paragraph.
How to Write the Introduction for NURS-FPX6011 Assessment 1 Evidence-Based Patient-Centered Concept Map
The introduction of the paper is the most crucial part as it helps to provide the context of your work, and will determine if the reader will be interested to read through to the end. You should start with a hook, which will help capture the reader’s attention. You should contextualize the topic by offering the reader a concise overview of the topic you are writing about so that they may understand its importance. You should state what you aim to achieve with the paper. The last part of the introduction should be your thesis statement, which provides the main argument of the paper.
How to Write the Body for NURS-FPX6011 Assessment 1 Evidence-Based Patient-Centered Concept Map
The body of the paper helps you to present your arguments and evidence to support your claims. You can use headings and subheadings developed in the paper’s outline to guide you on how to organize the body. Start each paragraph with a topic sentence to help the reader know what point you will be discussing in that paragraph. Support your claims using the evidence conducted from the research, ensure that you cite each source properly using in-text citations. You should analyze the evidence presented and explain its significance and how it connects to the thesis statement. You should maintain a logical flow between each paragraph by using transition words and a flow of ideas.
How to Write the In-text Citations for NURS-FPX6011 Assessment 1 Evidence-Based Patient-Centered Concept Map
In-text citations help the reader to give credit to the authors of the references they have used in their works. All ideas that have been borrowed from references, any statistics and direct quotes must be referenced properly. The name and date of publication of the paper should be included when writing an in-text citation. For example, in APA, after stating the information, you can put an in-text citation after the end of the sentence, such as (Smith, 2021). If you are quoting directly from a source, include the page number in the citation, for example (Smith, 2021, p. 15). Remember to also include a corresponding reference list at the end of your paper that provides full details of each source cited in your text. An example paragraph highlighting the use of in-text citations is as below:
The integration of technology in nursing practice has significantly transformed patient care and improved health outcomes. According to Smith (2021), the use of electronic health records (EHRs) has streamlined communication among healthcare providers, allowing for more coordinated and efficient care delivery. Furthermore, Johnson and Brown (2020) highlight that telehealth services have expanded access to care, particularly for patients in rural areas, thereby reducing barriers to treatment.
How to Write the Conclusion for NURS-FPX6011 Assessment 1 Evidence-Based Patient-Centered Concept Map
When writing the conclusion of the paper, start by restarting your thesis, which helps remind the reader what your paper is about. Summarize the key points of the paper, by restating them. Discuss the implications of your findings and your arguments. End with a call to action that leaves a lasting impact on the reader or recommendations.
How to Format the Reference List for NURS-FPX6011 Assessment 1 Evidence-Based Patient-Centered Concept Map
The reference helps provide the reader with the complete details of the sources you cited in the paper. The reference list should start with the title “References” on a new page. It should be aligned center and bolded. The references should be organized in an ascending order alphabetically and each should have a hanging indent. If a source has no author, it should be alphabetized by the title of the work, ignoring any initial articles such as “A,” “An,” or “The.” If you have multiple works by the same author, list them in chronological order, starting with the earliest publication.
Each reference entry should include specific elements depending on the type of source. For books, include the author’s last name, first initial, publication year in parentheses, the title of the book in italics, the edition (if applicable), and the publisher’s name. For journal articles, include the author’s last name, first initial, publication year in parentheses, the title of the article (not italicized), the title of the journal in italics, the volume number in italics, the issue number in parentheses (if applicable), and the page range of the article. For online sources, include the DOI (Digital Object Identifier) or the URL at the end of the reference. An example reference list is as follows:
References
Johnson, L. M., & Brown, R. T. (2020). The role of telehealth in improving patient outcomes. Journal of Nursing Care Quality, 35(2), 123-130. https://doi.org/10.1097/NCQ.0000000000000456
Smith, J. A. (2021). The impact of technology on nursing practice. Health Press.
NURS-FPX6011 Assessment 1 Evidence-Based Patient-Centered Concept Map Instructions
- Create a concept map graphic and write a 2-4 page narrative on the patient scenario presented in Assessment Case Study: Evidence-Based Patient-Centered Concept Map. Base your report on the information provided in the case study and your own research of 3-5 evidence-based resources.
Evidence-based practice is a key skill in the tool kit of the master’s-prepared nurse. Its goal is to ensure that health care practitioners are using the best available evidence to ensure that patients are receiving the best care possible (Godshall, 2020). In essence, evidence-based practice is all about ensuring quality care.
In this assessment, you will apply evidence-based practice and personalized care concepts to ensure quality care and improve the health of a single patient. The concept map that you will create is an example of a visual tool that you can use for patient and family education. Have a look at NURS-FPX6011 Assessment 2 Evidence-Based Population Health Improvement Plan.
Reference
Godshall, M. (2020). Fast facts for evidence-based practice in nursing (3rd ed.). Springer Publishing Company.
Scenario
The charge nurse at the wellness center has sent you an email to request that you review a patient file before the patient arrives at the clinic. She has asked you to put together a concept map for your patient’s care plan. The concept map is intended to help you think through the best strategy for your patient’s care and for subsequent use for patient education. In addition, the nurse needs a narrative report that describes your patient with up to five diagnoses, in order of urgency.
Your Role
You are a nurse at a community wellness center who has received a request for patient case review and preparation for an upcoming appointment.
Instructions
Review the Assessment Case Study: Evidence-Based Patient-Centered Concept Map media activity.
Create your concept map and narrative as separate parts of your document. Be sure to note where you must include your evidence-based support and clarify your strategies for communicating information to the patient and the patient’s family.
Integrate relevant evidence from 3–5 current scholarly or professional sources to support your assertions.
Part 1: Concept Map
- Develop a graphical concept map for the patient based on the best available evidence for treating your patient’s health, economic, and cultural needs.
- Many organizations use the spider style of concept maps (see the Taylor and Littleton-Kearney article for an example).
- The Assessment Case Study: Evidence-Based Patient-Centered Concept Map, which includes an example of a concept map, may help you prepare your assessment.
- If a particular style of concept map is used in your current care setting, you may use it in this assessment.
Part 2: Narrative Report
- Develop a narrative (2–4 pages) for your concept map.
- Analyze the needs of a patient and his or her family to ensure that the intervention in the concept map will be relevant and appropriate for their beliefs, values, and lifestyle.
- Consider how your patient’s economic situation and relevant environmental factors may have contributed to your patient’s current condition or could affect future health.
- Consider how your patient’s culture or family should inform your concept map.
- Determine the value and relevance of the evidence you used as the basis of your concept map.
- Explain why your evidence is valuable and relevant to your patient’s case.
- Explain why each piece of evidence is appropriate for the health issue you are addressing and for the unique situation of your patient and the family.
- Propose relevant and measurable criteria for evaluating the outcomes the patient needs to achieve.
- Explain why your proposed criteria are appropriate and useful measures of success.
- Explain how you will communicate specific aspects of the concept map to your patient and the family in an ethical, culturally sensitive, and inclusive way. Ensure that your strategies:
- Promote honest communications.
- Facilitate sharing only the information you are required and permitted to share.
- Are mindful of your patient’s culture.
- Enable you to make complex medical terms and concepts understandable to your patient and his or her family, regardless of language, abilities, or educational level.
Additional Requirements
- Organization: Use the following headings for your Diabetes Patient Concept Map assessment:
- Concept Map.
- Patient Needs Analysis.
- Value and Relevance of the Evidence.
- Proposed Criteria for Patient Outcome Evaluation.
- Patient and Family Communication Plan.
- Length: Your concept map should fit on one page (possibly a horizontal layout) and your narrative report will be 2–4 double-spaced pages, not including title and reference pages.
- Font: Times New Roman, 12 points.
- APA Format: Your title and reference pages must follow current APA format and style guidelines. The body of your paper does not need to conform to APA guidelines. Do make sure that it is clear, persuasive, organized, and well written, without grammatical, punctuation, or spelling errors. You also must cite your sources according to APA guidelines.
- Scoring Guide: Please review this assessment’s scoring guide. The requirements outlined above correspond to the grading criteria in the scoring guide, so be sure to address each point. In addition, you may want to review the performance-level descriptions for each criterion to see how your work will be assessed.
Competencies Measured
By successfully completing this assessment, you will demonstrate your proficiency in the course competencies through the following assessment scoring guide criteria:
- Competency 1: Apply evidence-based practice to plan patient-centered care.
- Design an individualized, patient-centered concept map, based upon the best available evidence for treating a patient’s specific health, economic, and cultural needs.
- Analyze the needs of a patient, and those of their family, to ensure that the intervention in the concept map will be relevant and appropriate for their beliefs, values, and lifestyle.
- Competency 3: Evaluate outcomes of evidence-based interventions.
- Propose relevant and measurable criteria for evaluating the outcomes the patient needs to achieve.
- Competency 4: Evaluate the value and relative weight of available evidence upon which to make a clinical decision.
- Determine the value and relevance of evidence used as the basis of a patient-centered concept map.
- Competency 5: Synthesize evidence-based practice and academic research to communicate effective solutions.
- Develop a strategy for communicating with patients and their families in an ethical, culturally sensitive, and inclusive way.
- Integrate relevant and credible sources of evidence to support assertions, correctly formatting citations and references using APA style.
NURS-FPX6011 Assessment 1 Evidence-Based Patient-Centered Concept Map Example
Part 2: Supporting the Concept Map
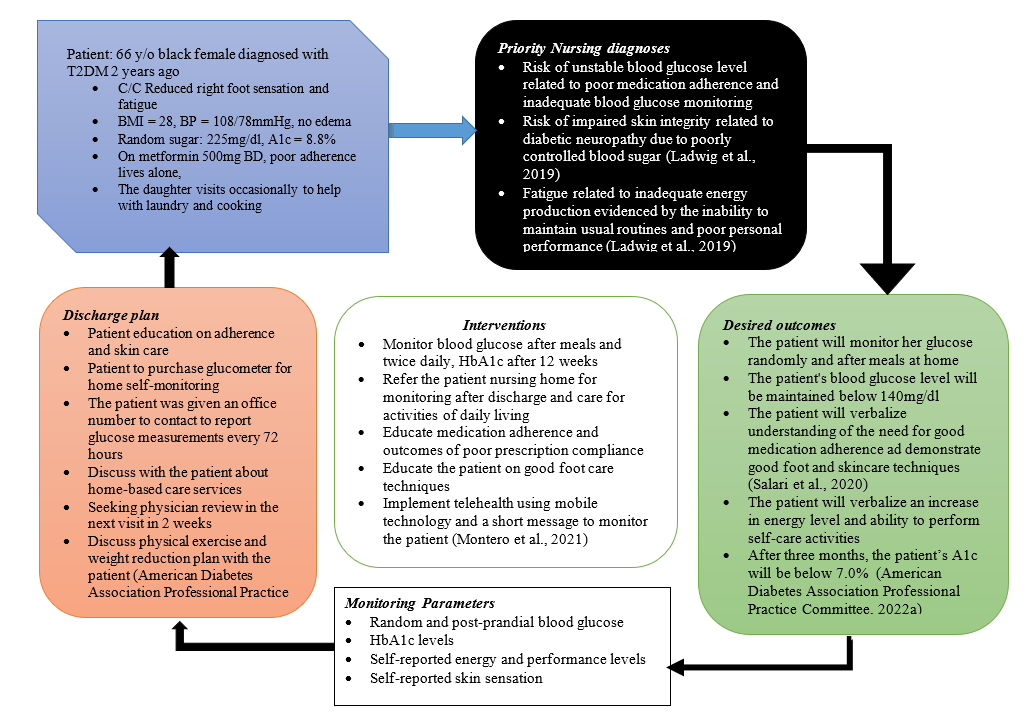
The development of this concept map was guided by the nursing process. This patient came into the office with a chief complaint of reduced sensation on the right foot that was on and off but mild in functional limitation. The assessment revealed no other symptoms related to renal, ophthalmic, gastrointestinal, or cardiac complications of diabetes. The purpose of this narrative review of the concept map is to describe how evidence-based practice influenced this concept map and care plan in terms of analysis of the patient’s needs, communication with the patient and her family, and the value of the evidence-based sources used.
Patient Needs Analysis
During this visit, the patient’s main concerns were the reduction of right lower limb and foot sensation and fatigue. On further probing, the assessment found that this patient’s compliance with her metformin has been erratic and her socioeconomic circumstances could have also contributed to her current situation. She has missed most of her doses in the past few months because her daughter, who used to remind her to take her pills, moved to another state for permanent employment and has been held up with work lately.
The patient is retired; thus, her primary source of income is through her son and daughter, who are both employed. Her children are both married but still find time to come and visit. This patient is a staunch Christian believer and she reports that her faith has kept her through to this time. This might have contributed to the reluctance to comply fully with her prescription. Nevertheless, this patient’s cultural and socioeconomic needs greatly influenced the development of this concept map and the care plan.
The patient lives alone; thus, this care plan instituted monitoring strategies to ensure that the patient achieves self-care by improving her fatigue. Priority was given to stabilizing blood sugar levels and improving adherence to ensure that her metabolic demands were met. Monitoring through telehealth and mobile technology was a vital part of this plan because it would enable remote management of the patient through enhanced follow-up after short time intervals. In the discharge plan, the patient was helped to create a plan that included an alarm to remind her about her medication time and times to record her blood glucose to report three days later.
The development of the patient was also influenced by her identity and cultural needs. As an African American, she is at risk of cardiovascular diseases such as heart failure. Therefore, an assessment of her blood pressure and cardiovascular complication, such as lower limb edema from heart failure and acute kidney injury, was justified for this patient. This patient is overweight (BMI=28), which adds to her cardiovascular risk. Therefore, the inclusion of exercise and a weight reduction plan through diet were discussed during a motivational interviewing session.
The interventions were driven at meeting care needs illustrated in the three priority diagnoses. Most of the desired outcomes of these interventions were intertwined and such that more than one intervention could be used to meet a single outcome. Therefore, I included the monitoring outcomes measurement parameters that would be discussed with the patient during every review session after every 72 hours. The patient’s family was included in this plan through her daughter, who accompanied her to the office. She desired to treat her mother from home even if it meant that the care costs would increase. Therefore, I added community resources such as home-based care interventions to improve this patient’s self-care at home.
Communication Strategies.
The communication plan with this patient and her family will involve both remote and face-to-face communication. Remote communication through telehealth would help monitor patient progress and scheduling appointments. After every four weeks, the patient would revisit the officer for physical assessment and face-to-face communication. To ensure that these communications were honest and productive.
The communication times would be scheduled and contents tailored to meet the patient’s care needs. The patient’s daily readings would be communicated through phone calls but charted on paper to be delivered during physical sessions. This would ensure that only important and useful is shared, but every detail is documented for monitoring and evaluation. The content of the communication with the patient and her family will be kept short and basic so that they would understand and follow through with her care.
Value and Relevance of Resources
Four evidence-based sources informed this care plan. These sources have different values and relevance to making the concept map. The annotated bibliography below explains how these sources were valuable ad relevant.
American Diabetes Association Professional Practice Committee. (2022a). 4. Comprehensive medical evaluation and assessment of comorbidities: Standards of Medical Care in diabetes—2022. Diabetes Care, 45(Supplement_1), S46–S59. https://doi.org/10.2337/dc22-s004
This source provided information on current evaluation and assessment strategies relevant to the nursing process. This piece of information was relevant to this patient’s case because it ensures that my care was multisystemic and, thus, holistic and patient-centered. This article provides level I evidence in the hierarchy of evidence because it contains evidence-based guidelines. The value of the information herein is critical to patient safety and quality of care.
American Diabetes Association Professional Practice Committee. (2022b). 5. Facilitating behavior change and well-being to improve health outcomes: Standards of Medical Care in diabetes—2022. Diabetes Care, 45(Supplement_1), S60–S82. https://doi.org/10.2337/dc22-s005
This resource was a peer review article that provided information on the current management of diabetes and the incorporation of mental health outcomes relevant to this patient. This piece of information was relevant to this patient’s case because it ensured that my care was multisystemic and, thus, holistic and patient-centered. This article provides level I evidence in the hierarchy of evidence because it contains evidence-based guidelines by a recognized and reputable organization, the American Diabetes Association.
Ladwig, G. B., Ackley, B. J., & Makic, M. B. F. (2019). Mosby’s guide to nursing diagnosis (6th ed.). Mosby.
This resource is a course book and a tertiary source of information. The content of this source is heterogeneous and sourced from different primary and secondary articles and guidelines. The quality of evidence in this resource is high but can’t be ranked in the hierarchy because this resource doesn’t contain a single topic of information. This resource was vital in needs assessment and making priority diagnoses for this patient that are related to NANDA diagnoses. This information was also important for goal setting for the care of this patient.
Montero, A. R., Toro-Tobon, D., Gann, K., Nassar, C. M., Youssef, G. A., & Magee, M. F. (2021). Implications of remote monitoring Technology in Optimizing Traditional Self-Monitoring of blood glucose in adults with T2DM in primary care. BMC Endocrine Disorders, 21(1), 222. https://doi.org/10.1186/s12902-021-00884-6
This source of information was the primary source with the information I used in the selection of the best and most appropriate technology for communication to meet this patient’s needs. The use of technology would ensure self-monitoring of glucose by this patient and this would improve outcomes. This source is level II evidence because it was from a comparative experimental study with no randomization.
Salari, N., Hosseinian-Far, A., Hosseinian-Far, M., Kavoussi, H., Jalali, R., Vaisi-Raygani, A., Rasoulpoor, S., Rasoulpoor, S., Mohammadi, M., & Shabani, S. (2020). Evaluation of skin lesions in diabetic patients: a systematic review and meta-analysis. Journal of Diabetes and Metabolic Disorders, 19(2), 1909–1916. https://doi.org/10.1007/s40200-020-00629-7
The value of this article in the management of this patient is high because it is a level-I evidence source that addresses this patient’s chief complaint. This source is a systemic review with meta-analyses; thus, it provides the highest level of evidence (Melnyk & Fineout-Overholt, 2023). This article provides information about current best practices regarding skin care among diabetic patients. Therefore, it is relevant to this patient’s case.
The above five sources are credible because they meet the CRAAP criteria for credibility. The CRAAP credibility test is an acronym that stands for currently, relevance, accuracy, authoritativeness, and purpose. I used sources published within the last five years, thus current. These sources were published by an expert in nursing and medical fields and are thus authoritative. The purpose and relevance of the sources had been annotated earlier.
Conclusion
The concept map presented summarized the patient assessment findings, presented three priory nursing diagnoses and elaborated a care plan for the patient. The desired outcomes of the patient care plan were based on an assessment of the patient’s needs. These needs were related to the patient’s current social, economic, cultural, and self-care status. This plan was evidence based because the information that guided its development was derived from five credible sources.
References
American Diabetes Association Professional Practice Committee. (2022a). 4. Comprehensive medical evaluation and assessment of comorbidities: Standards of Medical Care in diabetes—2022. Diabetes Care, 45(Supplement_1), S46–S59. https://doi.org/10.2337/dc22-s004
American Diabetes Association Professional Practice Committee. (2022b). 5. Facilitating behavior change and well-being to improve health outcomes: Standards of Medical Care in diabetes—2022. Diabetes Care, 45(Supplement_1), S60–S82. https://doi.org/10.2337/dc22-s005
Ladwig, G. B., Ackley, B. J., & Makic, M. B. F. (2019). Mosby’s guide to nursing diagnosis (6th ed.). Mosby.
Melnyk, B. M., & Fineout-Overholt, E. (2023). Evidence-based practice in nursing & healthcare: A guide to best practice (5th ed.). Wolters Kluwer Health.
Montero, A. R., Toro-Tobon, D., Gann, K., Nassar, C. M., Youssef, G. A., & Magee, M. F. (2021). Implications of remote monitoring Technology in Optimizing Traditional Self-Monitoring of blood glucose in adults with T2DM in primary care. BMC Endocrine Disorders, 21(1), 222. https://doi.org/10.1186/s12902-021-00884-6
Salari, N., Hosseinian-Far, A., Hosseinian-Far, M., Kavoussi, H., Jalali, R., Vaisi-Raygani, A., Rasoulpoor, S., Rasoulpoor, S., Mohammadi, M., & Shabani, S. (2020). Evaluation of skin lesions in diabetic patients: a systematic review and meta-analysis. Journal of Diabetes and Metabolic Disorders, 19(2), 1909–1916. https://doi.org/10.1007/s40200-020-00629-7
